So many TMD patients go doctor to dentist, to specialist, to chiropractor, osteopath, acupuncture, massage, and everyone they see has an opinion, and has a splint, and the patient spends a lot of money and gets frustrated. You see a lot of it on chat groups, people complaining about going to all these professionals and not getting anywhere with symptom resolution. And all these doctors, dentists, all mean well, and want to resolve these cases, so what happens is our profession starts to blame it on the patient and say it’s in their head and they medicate. Prescriptions for pain, prescriptions for anti-depressants, for sedatives but none of them address the actual root cause of their pain.
Difference Between a Splint & a Nightguard & an Orthotic
Patients tell me all the time: I’ve had 3 splints and none of them work. Or, my last dentist made me a nightguard but it makes my pain worse so I don’t wear it. Here is the problem: the dentist takes impressions (or scans) and sends to a lab and makes an upper splint, or a nightguard, and delivers to the patient, and the patient goes home and nothing happens, or gets worse. Dental school doesn’t teach us to take proper bite relationship records, especially in a TMD patient. What they teach is to take an impression of upper and lower teeth, then the lab opens the bite the way they see fit, and they make the splint but that doesn’t take the 3-dimensional position and behaviour of the jaw, especially in a TMD patient.
What dentists and patients all need to understand, and nobody talks about this, is that splints/nightguards are like shoes. You need different shoes for different situations. If you are going to a big function, you need beautiful dress shoes with a nice heal, maybe high heal, or pointed toe. If you are going running, those same shoes you just wore to the function wouldn’t work; try running in high heels held to your foot only by a strap! What if you had to trek through the woods in the snow? Which shoes would work best for this occasion?
Splints and nightguards and even orthotics, are all basically the same thing – an acrylic dental appliance made to be worn on upper or lower teeth to do something. But it’s in the “something” that dentists go wrong. They make a shoe for the wrong situation. It’s all in the 3-dimensional design. Where you put the support (as in, the “high heel” or lack of) in 3 dimensions is the key to making the appliance.
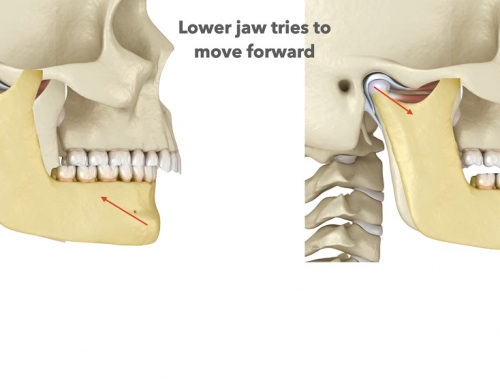
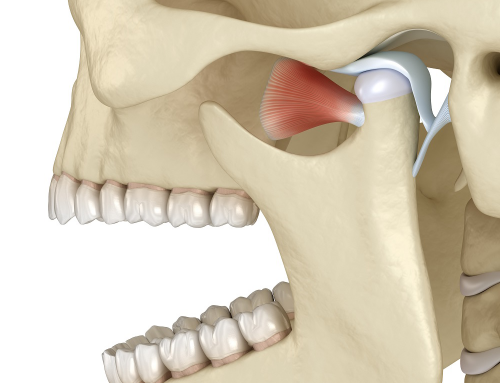
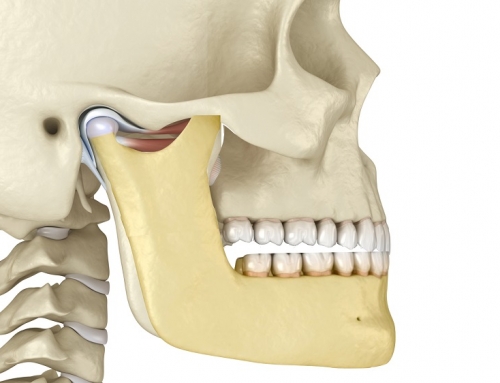
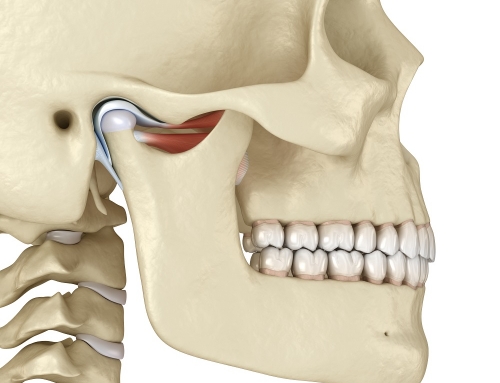
But wait, there is more! Not only is the design a problem in 99% of splints or nightguards made, there is a general lack of understanding regarding what resolves TMD symptoms to begin with. Most splints are upper splints, but in 75% of TMD cases, the patient is retruded (the mandible is further back than it should be) and, in general, upper splints tend to distalize the mandible (retrude it), making TMD symptoms worse not better. Other splints are soft (or become soft when heated in water, or in mouth); you can’t use a soft splint in a clencher – you will make them clench more. Most are also flat plane on the surface, but flat plane splints/nightguards do not effectively address the requirements of maintaining optimal muscle position. Simple nightguards with a flat plane can be used to manage some conditions where symptoms are minimal or non-existent. But when joint degeneration or derangement exists (in a TMD patient), the jaw joint needs to be supported in its optimal position in order to heal and resolve symptoms. Flat plane splints usually position the jaw in a posterior position. This is because the hyperactivity of muscles over-ride the flat plane of the splint and do not help achieve a physiologic jaw relationship. Since they do not establish a physiologic occlusal jaw relationship, they often do not help support optimal physiotherapy, chiropractic alignment, and any other therapy aimed at symptom resolution. What’s missing is the proper physiologic occlusal support.
3 Dimensional Design is Key
The muscles of mastication (chewing) have proprioceptive mechanisms built in within them, and “seek” tooth contact that allows them to rest in their Optimal Physiologic Position OPP). This is the ideal comfortable position for these muscles in all dimensions, including sagittal, frontal, and horizontal. Torque of the mandible (lower jaw) also needs to be included in order to allow the muscles to function optimally. When the muscles are shortened, or pulled back, the contraction results in pain and other symptoms. When the contraction becomes severe and causes hyperactivity of the temporalis and masseter muscles, this results in worn posterior second molars and worn and rubbed out splints in the posterior region over time.
An anatomically correct orthotic that includes correct anterior and posterior vertical dimension of the jaw and supports the muscles, is required for TMD patients. This is not taught in dental school; in fact, it’s not taught almost anywhere. But it’s the physiologic design and anatomical form is the key to any appliance if one’s goals and objectives is to bring the muscles to their neutral and relaxed functional position effectively. When muscles are strained, the jaw position and tooth relationships change, and this is a critical factor to understand when treating TMJ Dysfunction. Building in anatomy and chewing movements into the orthotic appliance that puts the patient in the OPP is key to helping TMD patients heal quickly through phase I of their treatment.